Introduction
I trained in gastrointestinal endoscopy at NTT Medical Center Tokyo, a high-volume center in Japan performing over 1,000 endoscopic submucosal dissections (ESDs) annually. The hospital also served as an international training site, hosting 62 overseas trainees in 2024. Since September 2024, I have been practicing endoscopy at Haukeland University Hospital in Norway. This essay outlines my training at NTT Medical Center Tokyo and compares it with current practices in Norway.
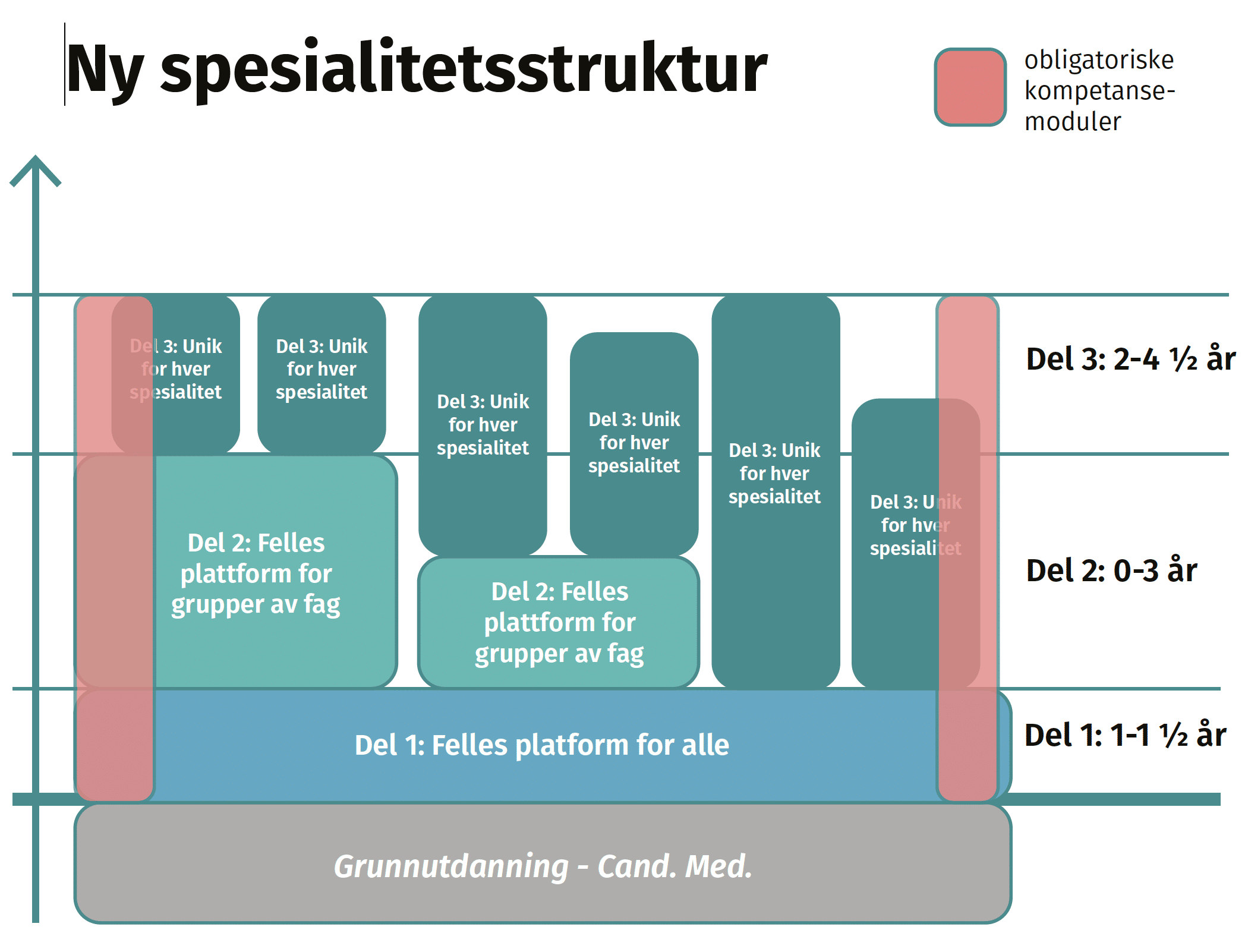
Comparison of Endoscopic Training Systems in Norway and Japan
Norway has developed a nationwide structure for endoscopy education through Endoskopiskolen, offering organized training for both endoscopists and nursing staff. The system includes specific programs to train future trainers. The effectiveness of such programs has been demonstrated in previous studies [1].
Colonoscopy insertion methods are unified across institutions, reducing instructional variability and trainee confusion. Validated tools are used to assess technical skills, supported by the national Gastronet registry, which promotes quality improvement.
Japan also operates a national registry, the Japan Endoscopy Database (JED), which gathers extensive clinical data. However, a unified, validated training and assessment system has not yet been implemented [2]. Training methods— for instance with regards to colonoscope insertion techniques— differ widely between institutions, as each has developed its own style [3]. Most programs are physician-focused, with limited inclusion of nurses or team-based instruction.
ESD Training at NTT Medical Center Tokyo
At NTT Medical Center Tokyo, a high-volume ESD center, training focuses on developing endoscopists who can perform ESD independently. Prior to commencing ESD training, the physician is trained in colonoscopic techniques, focusing on fundamentals such as loop avoidance and management as described by Professor Shin-ei Kudo using a technique referred to as axis keeping shortening. This is combined with training scope handling dexterity. Even experienced endoscopists relearn our methods from scratch. Only after mastering fundamental colonoscopy at a sufficient level (as presented in table 1) can the physician commence their ESD training; physicians are often able to achieve high self-completion rates even during their initial colorectal ESD cases under supervision following sound endoscopic training [4]. After completing 40 colorectal ESD cases, trainees proceed to 40 cases each of gastric and esophageal ESD before performing independent procedures. The overall training pathway is outlined (Figure 1).
| Parameter | Threshold |
|---|---|
| Cecal intubation rate | ≥ 98% |
| Cecal intubation without loop formation | ≥ 60% |
| Mean insertion time | ≤ 7 minutes |
| Mean total examination time (incl. polypectomy) | ≤ 20 minutes |
| Adenoma Detection Rate | ≥ 40% |
| Proficiency in magnifying endoscopy | Required |
| EMR (Endoscopic Mucosal Resection) competency | Required |
Table 1: Colonoscopy criteria for progression to ESD
Conclusion
While national systems vary, individual institutions can still play a crucial role in shaping effective endoscopic training through structured local programs. In Norway, advanced endoscopy training programs, including those for procedures such as ESD, are also being developed. Sharing experiences across systems may contribute to creating more effective training environments for the future.